Mouth swelling can range from a minor inconvenience to a potentially life-threatening medical emergency. Understanding when severe mouth swelling requires immediate attention is crucial for protecting your health and preventing serious complications. This comprehensive guide will help you identify warning signs, understand underlying causes, and know when to seek emergency care for swollen mouth conditions.
Table of Contents
Understanding Mouth Swelling and Its Causes
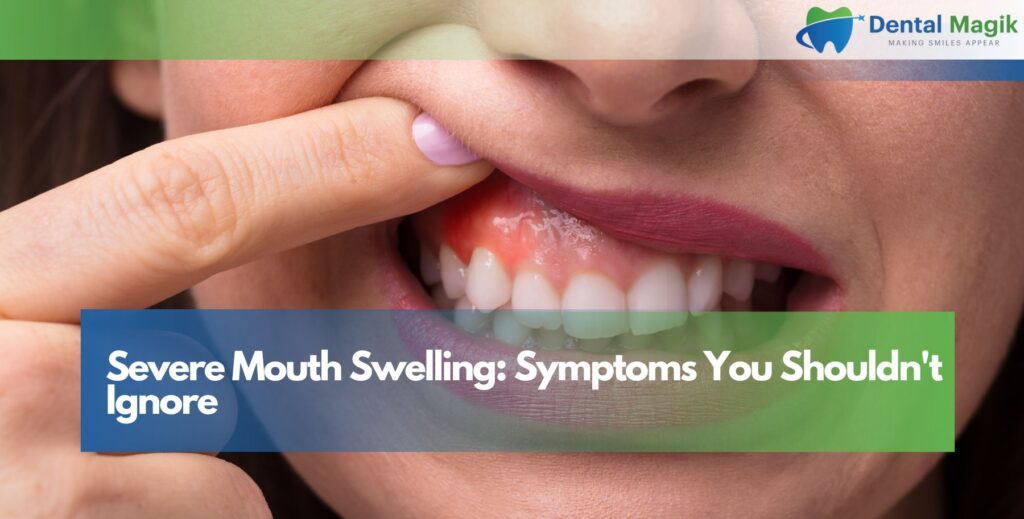
Mouth swelling occurs when tissues in and around the oral cavity become inflamed due to various factors including infections, allergic reactions, trauma, or underlying medical conditions. The swelling can affect different areas including the lips, gums, tongue, cheeks, and throat. While mild swelling may resolve on its own, severe mouth swelling often indicates a serious condition requiring immediate medical intervention.
Bacterial infections are among the most common causes of significant oral swelling. These infections can originate from tooth abscesses, gum disease, or oral wounds that become contaminated. When bacteria multiply rapidly, they can cause intense inflammation and swelling that spreads beyond the initial infection site.
Allergic reactions can also cause sudden and severe mouth swelling. Food allergies, medication reactions, or exposure to environmental allergens can trigger angioedema, a condition characterized by deep swelling of the face, lips, and mouth tissues. This type of swelling can develop rapidly and may compromise breathing if it affects the throat and airway.
Recognizing Dangerous Symptoms
Identifying critical warning signs of severe mouth swelling can be life-saving and prevents serious complications from developing. Understanding the difference between mild swelling and emergency situations helps patients make informed decisions about seeking immediate care. Recognizing these dangerous symptoms early enables prompt treatment and significantly improves outcomes for patients experiencing oral emergencies.
Immediate Emergency Signs
Certain symptoms accompanying mouth swelling indicate a medical emergency requiring immediate attention. Difficulty breathing or shortness of breath suggests that the swelling may be affecting your airway, which can be life-threatening. Difficulty swallowing or a feeling that your throat is closing also requires emergency care.
Rapid onset swelling that develops within minutes or hours, especially when accompanied by hives, itching, or dizziness, may indicate a severe allergic reaction or anaphylaxis. This condition can be fatal without prompt treatment and requires immediate emergency medical intervention.
Progressive Warning Signs
Severe pain that worsens rapidly, high fever above 101°F, and swelling that spreads to the neck or affects your ability to open your mouth are serious warning signs. Difficulty speaking clearly, drooling, or inability to swallow saliva normally also indicate that the swelling may be interfering with normal oral function.
Red streaking from the swollen area toward the neck or other parts of the face suggests that an infection may be spreading through the lymphatic system. This condition, known as lymphangitis, requires immediate antibiotic treatment to prevent sepsis.
Common Causes of Severe Mouth Swelling
Understanding the underlying causes of severe mouth swelling helps patients identify potential risk factors and seek appropriate treatment. Different conditions require specific approaches to management and treatment, making accurate diagnosis essential. Knowledge of these common causes enables better prevention strategies and helps patients communicate effectively with healthcare providers about their symptoms and concerns.
Dental Abscesses
Dental abscesses are localized infections that develop when bacteria invade the pulp of a tooth or the tissues surrounding the tooth root. These infections can cause significant facial swelling that may extend from the affected tooth to the cheek, jaw, or neck. Abscessed teeth often cause throbbing pain and can lead to serious complications if left untreated.
The swelling from a dental abscess typically develops gradually but can become severe enough to affect eating, speaking, and sleeping. In some cases, the infection can spread to deeper facial tissues, creating a condition called cellulitis that requires aggressive treatment.
Cellulitis and Deep Tissue Infections
Oral cellulitis is a serious bacterial infection that affects the deeper layers of skin and soft tissues in the mouth and face. Unlike superficial infections, cellulitis spreads rapidly through tissue planes and can cause extensive swelling that feels firm and warm to the touch.
Ludwig’s angina is a particularly dangerous form of cellulitis that affects the floor of the mouth and can rapidly compromise the airway. This condition causes severe swelling under the tongue and in the neck area, potentially pushing the tongue upward and backward, blocking the airway.
Allergic Reactions and Angioedema
Angioedema causes deep swelling in the lips, face, and mouth tissues due to allergic reactions. This condition can be triggered by foods, medications, insect stings, or environmental allergens. The swelling typically affects one side of the face more than the other and can develop within minutes of exposure to the allergen.
Hereditary angioedema is a rare genetic condition that causes recurrent episodes of severe swelling without an obvious allergic trigger. These episodes can affect the mouth, face, hands, feet, and potentially the throat and airway.
Treatment Approaches for Severe Mouth Swelling
Effective treatment of severe mouth swelling requires rapid assessment and appropriate intervention based on the underlying cause and severity of symptoms. Treatment strategies range from emergency life-saving measures to targeted dental procedures and antibiotic therapy. Understanding available treatment options helps patients prepare for procedures and actively participate in their recovery and ongoing oral health maintenance.
Emergency Medical Care
Severe mouth swelling that affects breathing or swallowing requires immediate emergency treatment. Emergency medical professionals may administer epinephrine for allergic reactions, corticosteroids to reduce inflammation, and antihistamines to counteract allergic responses.
In cases where airway obstruction is imminent, emergency procedures such as intubation or tracheostomy may be necessary to maintain breathing. Intravenous antibiotics are typically administered for severe bacterial infections causing the swelling.
Dental Treatment
When mouth swelling results from dental infections, prompt dental treatment is essential. This may include root canal therapy to treat infected teeth, tooth extraction for severely damaged teeth, or incision and drainage of abscesses to remove infected material.
Oral surgeons may need to perform more complex procedures for deep facial infections or when swelling affects multiple tissue planes. These procedures often require general anesthesia and hospitalization for monitoring and intravenous antibiotic administration.
Medication Management
Antibiotic therapy is the cornerstone of treatment for bacterial infections causing mouth swelling. The choice of antibiotic depends on the suspected bacteria and the severity of the infection. Broad-spectrum antibiotics are often used initially until culture results can guide more specific treatment.
Anti-inflammatory medications such as corticosteroids can help reduce swelling and inflammation, particularly in cases of allergic reactions or autoimmune conditions. Pain management with appropriate medications is also important for patient comfort during treatment.
Prevention and Risk Reduction
Proactive prevention strategies significantly reduce the risk of developing severe mouth swelling and associated complications. Comprehensive oral health maintenance, allergy management, and lifestyle modifications work together to minimize infection risk and inflammatory responses. Implementing these preventive measures helps patients maintain optimal oral health while avoiding potentially dangerous swelling episodes that require emergency intervention.
Maintaining Oral Health
Preventing severe mouth swelling begins with excellent oral hygiene and regular dental care. Brushing twice daily, flossing regularly, and using antimicrobial mouthwash help prevent bacterial infections that can lead to swelling and abscesses.
Regular dental checkups allow for early detection and treatment of dental problems before they progress to serious infections. Professional dental cleanings remove bacterial buildup that can contribute to gum disease and other oral infections.
Managing Allergies
Individuals with known allergies should avoid trigger substances and carry emergency medications such as epinephrine auto-injectors when prescribed. Allergy testing can help identify specific triggers, allowing for better avoidance strategies.
Medical alert jewelry or cards can inform emergency responders about serious allergies or medical conditions that might cause mouth swelling, ensuring appropriate treatment is provided quickly.
Lifestyle Modifications
Tobacco cessation is crucial as smoking and tobacco use increase the risk of oral infections and impair healing. Stress management and adequate sleep support immune system function, helping the body fight off infections that could cause mouth swelling.
Maintaining good overall health through proper nutrition, regular exercise, and management of chronic conditions like diabetes also helps prevent oral health problems that can lead to severe swelling.
When to Seek Professional Help
Knowing when to seek professional medical or dental care for mouth swelling is crucial for preventing complications and ensuring optimal treatment outcomes. Different severity levels require varying degrees of urgency, from routine dental consultations to emergency interventions. Understanding these distinctions helps patients make informed decisions and avoid potentially dangerous delays in receiving appropriate medical care.
Urgent Care Situations
Seek immediate medical attention for mouth swelling accompanied by difficulty breathing, difficulty swallowing, high fever, rapid onset, or spreading redness. These symptoms may indicate serious conditions requiring emergency treatment.
Severe pain that doesn’t respond to over-the-counter medications, swelling that prevents normal mouth opening, or inability to eat or drink also warrant urgent medical evaluation.
Follow-Up Care
After treatment for severe mouth swelling, follow-up care is essential to ensure complete resolution and prevent recurrence. This may include continued antibiotic therapy, wound care, and monitoring for complications.
Allergy evaluation may be recommended for individuals who experienced swelling due to allergic reactions, helping identify triggers and develop prevention strategies.
Conclusion
Severe mouth swelling is a serious condition that requires prompt recognition and appropriate treatment. Understanding the warning signs, potential causes, and available treatments empowers individuals to seek timely care and avoid dangerous complications. Early intervention is key to preventing minor problems from becoming life-threatening emergencies.
If you experience severe mouth swelling or have concerns about oral health conditions, contact a qualified Dentist in East Brunswick, NJ immediately for professional evaluation and treatment. Don’t ignore symptoms that could indicate a serious condition requiring urgent care.
Frequently Asked Questions
When to worry about mouth swelling?
You should worry about mouth swelling when it’s accompanied by difficulty breathing, difficulty swallowing, high fever, rapid onset (developing within hours), severe pain, or swelling that spreads to your neck or affects your ability to open your mouth. Red streaking from the swollen area or inability to swallow saliva are also serious warning signs requiring immediate medical attention.
How to know if a mouth infection is serious?
A mouth infection is serious if it causes high fever (over 101°F), severe facial swelling, difficulty swallowing, trismus (inability to open mouth), rapid spreading of symptoms, or systemic symptoms like chills, nausea, or confusion. Cellulitis with red, warm, firm swelling or abscess formation also indicates a serious infection requiring prompt treatment.
What are the serious mouth conditions?
Serious mouth conditions include Ludwig’s angina (deep neck infection), orbital cellulitis, cavernous sinus thrombosis, necrotizing fasciitis, severe angioedema, oral cancer, osteomyelitis (bone infection), and sepsis from dental infections. These conditions can be life-threatening and require immediate medical intervention, often including hospitalization and intravenous antibiotics.
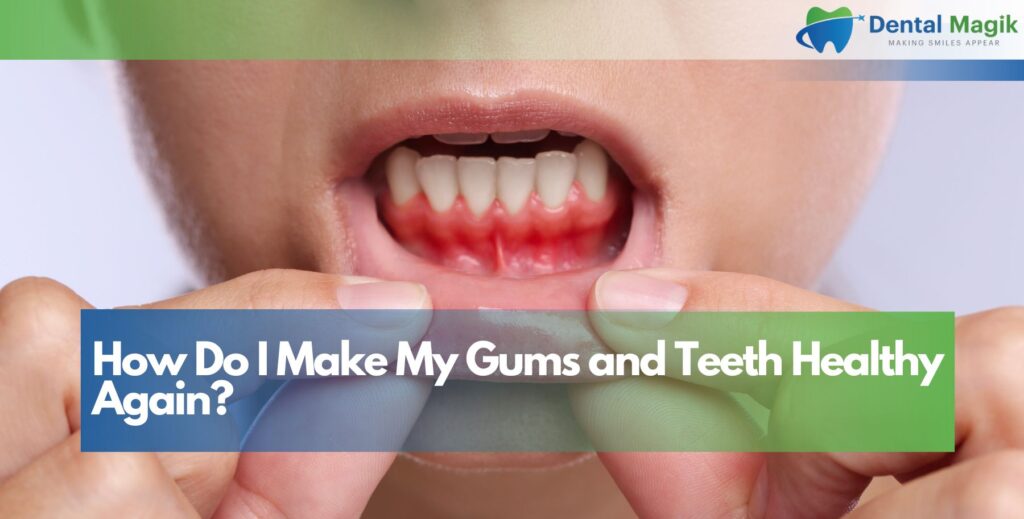
What causes swollen gums in children?
Swollen gums in children are commonly caused by poor oral hygiene, gingivitis, teething, viral infections like herpes simplex, hand-foot-mouth disease, bacterial infections, allergic reactions to foods or medications, mouth breathing, or orthodontic irritation. More serious causes include leukemia, vitamin deficiencies, or immune system disorders that require professional evaluation.
How do you know if swollen gums are serious?
Swollen gums are serious if accompanied by high fever, severe pain, bleeding that won’t stop, pus discharge, loose teeth, difficulty eating, swelling spreading to face or neck, persistent bad breath, or systemic symptoms. Chronic swelling lasting more than two weeks, ulcerations, or white patches on gums also require professional dental evaluation.
Is it safe to ignore inflamed gums?
No, it’s not safe to ignore inflamed gums as they can progress to serious periodontal disease, tooth loss, abscess formation, and systemic infections. Untreated gum inflammation can lead to periodontitis, which has been linked to heart disease, diabetes complications, and stroke. Early treatment of gingivitis is much more effective than treating advanced periodontal disease.
What happens if gum inflammation is untreated?
Untreated gum inflammation progresses to periodontitis, causing gum recession, bone loss, tooth mobility, and eventual tooth loss. The bacteria can enter the bloodstream, potentially causing endocarditis, pneumonia, or sepsis. Chronic inflammation may worsen diabetes, heart disease, and pregnancy complications, while deep periodontal pockets can harbor dangerous bacteria resistant to treatment.
How do dentists treat inflammation?
Dentists treat gum inflammation through professional cleaning, scaling and root planing (deep cleaning), antibiotic therapy, antimicrobial rinses, and laser therapy. Severe cases may require periodontal surgery, bone grafts, or guided tissue regeneration. Treatment also includes oral hygiene education, smoking cessation counseling, and maintenance therapy to prevent recurrence of inflammation.
Do you need antibiotics for gum inflammation?
Antibiotics for gum inflammation are typically needed only in severe cases with acute infection, abscess formation, systemic symptoms, or when scaling and root planing alone is insufficient. Topical antibiotics like chlorhexidine may be used for localized inflammation, while systemic antibiotics are reserved for aggressive periodontitis, compromised immune systems, or spreading infections requiring more intensive treatment.